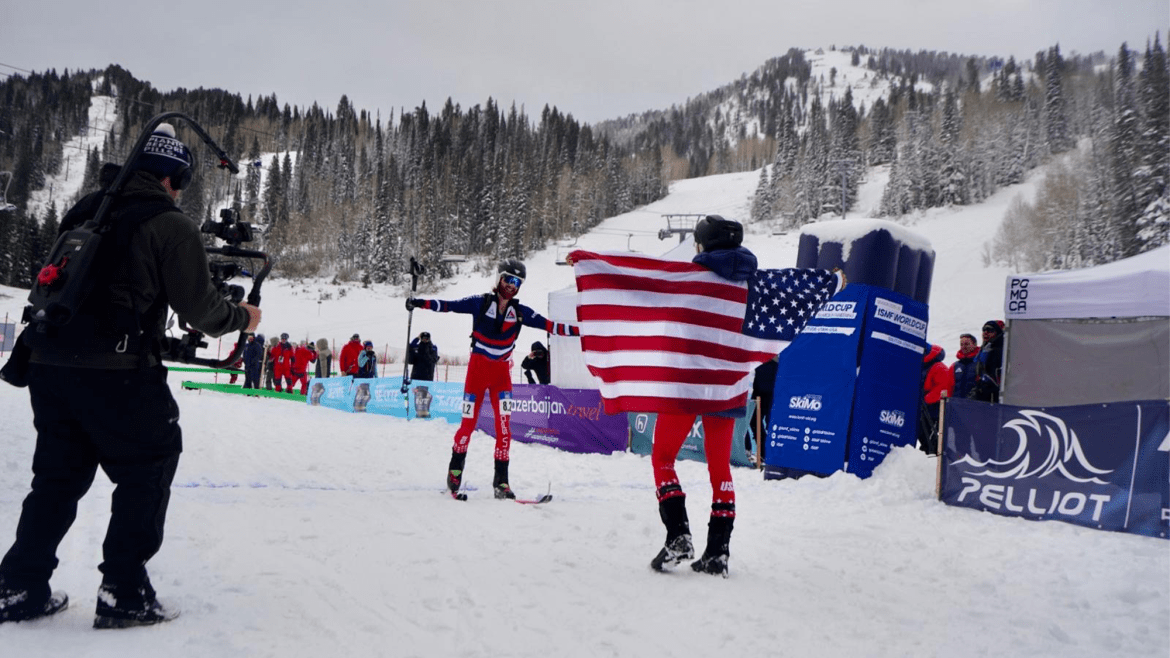
Olympic skimo is a spectacle. Appearing at the Games for the first time, skimo, short for ski mountaineering, grew from a long tradition of scaling mountains on skis—sometimes for hours on end—for the reward of gliding down, preferably through untracked powder. But at the Olympics, it will involve sprints of approximately three and a half minutes. First, athletes ascend a steep slope on skis outfitted with special fabric strips called “skins,” which prevent them from sliding backwards down the hill. Then they throw their skis on their back and hike in ski boots, put their skis back on for a final ascent, and finally peel off their skins to race downhill.
The events will include a mixed-gender skimo relay—“contrived for the Olympic field,” Sarah Cookler, the head of sport for USA Skimo, the sport’s American governing body, told me. Each team will include one man and one woman, each of whom will run the course twice. Anna Gibson and Cam Smith, both making their Olympic debuts, will represent Team USA.
It’s only fitting that such a new sport should debut on the world stage with a format that’s newly popular. Mixed-gender events, in which each team consists of a set number of men and women, have long had a place at the Olympics: Mixed-pairs figure skating and tennis were each introduced to the Games more than a century ago. But recently, such events have been growing in number as part of a deliberate effort to bring more attention to women’s sports. At Milan Cortina, every major sport category but ice hockey features mixed-gender events.
Women participated in the first Winter Olympics, in Chamonix in 1924, but only in figure skating. Women’s speed-skating exhibitions were included in the 1932 Olympics, but no medals were awarded. In 1936, women competed in alpine skiing, but they weren’t allowed in cross-country until 1952. Since then, the Winter Olympics have slowly been approaching a sort of parity, with women participating in an ever-growing number of events once considered too difficult, dangerous, or scandalous for them.
The International Olympic Committee is advertising the 2026 Games as “the most gender-balanced Olympic Winter Games in history.” That’s based on the fact that women will represent 47 percent of athletes participating and compete in 53 percent of all events; this Olympics is also the first where male and female cross-country skiers are competing at the same distances. But in terms of viewership and publicity, the many mixed-gender events may do more to raise the profile of female athletes than women’s events alone.
Women’s sports, including skimo, tend to attract far fewer spectators than men’s sports do. The mixed-gender relay can help bridge this gap, Smith told me, because in events that feature both men and women, viewers are positioned to watch everyone compete. And if the mixed-gender events allow spectators to get to know more female athletes, that could translate into more people watching the women’s stand-alone events. The IOC is leaning into these events: The Los Angeles Games in 2028 will feature 25 mixed-gender events, including new ones in golf, rowing, and artistic gymnastics.
Gibson told me she’s grown accustomed to elite sport spaces separating men and women as much as possible in the name of equity. She’s also a world-class trail runner and accomplished gravel-bike racer, and in those sports, “the talk has been all about giving women their own start in order to elevate women’s competition rather than having women be buried in the men’s field,” she said. Separate men’s and women’s fields have long been the default in most sports, and for good reason: If women had to compete directly with men, they would rarely have a chance to win. But bringing women and men together in competitions that include both gives women their own space and attention while including all the sport’s athletes within one community. It creates “a lot of camaraderie,” Gibson said, and in her experience, adds to the excitement among spectators.
Women, of course, face many obstacles in sport that cannot be solved by the addition of a few mixed-gender Olympic events. Across sports, male athletes are generally paid more than their female counterparts. In skimo, prize money is equal at the sport’s World Cup, but some other races still have unequal payouts, Cookler said. (Gibson said she avoids those.) Women athletes are still sometimes subjected to sexual harassment and abuse, even on the Olympic level. The Winter Olympics still include one event in which women are not allowed to compete at all—Nordic combined, which consists of ski jumping and cross-country skiing. (The IOC is already considering dropping Nordic combined altogether because of low participation and spectator interest; an IOC spokesperson told me the event “will undergo a full evaluation” following this year’s Olympics, and reiterated the committee’s commitment to gender equality.)
And mixed-gender formats can still be subject to unequal dynamics. Biathlon, a Winter Olympics event that combines cross-country skiing and target shooting, has used the mixed-gender relay format since the 2014 Olympics in Sochi. (Biathlon and luge were the first sports to introduce a mixed-gender format to the Winter Games since figure skating and ice dancing in the 20th century.) But “women always went first in our mixed-gender relays, and people felt it was unfair that a woman could never be the anchor,” Joanne Reid, a three-time Olympian who competed for Team USA last week, told me. In 2019, the sport’s governing body restructured the order of the competition so that the gender of the anchor rotates.
Even as mixed-gender events become more common, skimo’s inclusion in future Olympics is not assured. It’s in the 2026 Olympics because the organizers of this year’s Games proposed it; to continue competing, skimo athletes will need organizers at the next venues to propose its inclusion too. Skimo enthusiasts expect this to happen and hope future Olympics will include events that are longer and more representative of the sport’s origins. “Nobody got into skimo to do the sprint relay,” Smith said. But as he began training for the event, he enjoyed it more than he expected. “It’s really fun because we are accountable to each other,” he said. “I’m racing all out because I know that she’s doing the same for me.”