A year after the Trump administration began the dismantlement of USAID, it is initiating a new round of significant cuts to foreign assistance. This time, programs that survived the initial purge precisely because they were judged to be lifesaving are slated for cancellation.
According to an internal State Department email obtained by The Atlantic, the administration will soon end all of the humanitarian funding it is currently providing as part of a “responsible exit” from seven African nations, and redirect funding in nine others. Aid programs in all of these countries had previously been up for renewal from now through the end of September but will instead be allowed to expire. Each of them is classified as lifesaving according to the Trump administration’s standards.
The administration had already canceled the entire aid packages of two nations, Afghanistan and Yemen, where the State Department said terrorists were diverting resources. The new email, sent on February 12 to officials in the State Department’s Bureau of African Affairs, makes no such claims about the seven countries now losing all U.S. humanitarian aid: Burkina Faso, Cameroon, Malawi, Mali, Niger, Somalia, and Zimbabwe. Instead, according to the email, these projects are being canceled because “there is no strong nexus between the humanitarian response and U.S. national interests.” (The nine countries eligible for redirected funding are Ethiopia, the Democratic Republic of the Congo, the Central African Republic, Kenya, Mozambique, Nigeria, Uganda, South Sudan, and Sudan.)
A spokesperson for the State Department told me in an email that “as USAID winds down, the State Department is responsibly moving programming onto new mechanisms” with “longer periods of performance and updated award and oversight terms.” The State Department has recently begun signing health-financing agreements with some African governments—including Cameroon and Malawi, as well as five of the nine countries eligible for redirected funding—that will go into effect later this year. These agreements focus on strengthening health systems and containing infectious diseases but don’t seem to address the hunger or displacement crises that aid groups are fighting in these countries. The department’s internal email notes that aid projects in the nine eligible countries will be able to receive U.S. assistance via a United Nations program. But aid groups in at least one of those countries have already lost their U.S. funding, and much remains unknown about if and when additional support might come. The State Department spokesperson, who did not provide their name, offered no further specifics when asked.
As I wrote earlier this month, under Donald Trump, the U.S. has adopted an “America First” approach to foreign aid, in which many humanitarian projects are selected based not on need but on what the administration might receive in return. This latest aid purge appears to be following that pattern. Across the seven countries barred from U.S. aid, at least 6.2 million people are facing “extreme or catastrophic conditions,” according to the UN. But they have little to offer the U.S. in return for help. In other cases, the State Department has restored or offered aid in exchange for desirable mineral rights, or as payment for agreeing to accept U.S. deportees. Six of the seven countries mine comparatively few minerals that the Trump administration needs to fuel the AI boom. And only one, Cameroon, appears to have accepted a handful of deportees.
[Read: The logical end point of ‘America First’ foreign aid]
The email also confirms that the U.S. will no longer allow American taxpayer dollars to flow to these seven countries through the UN’s Office for the Coordination of Humanitarian Affairs, or OCHA. Previously, the U.S. placed a significant amount of money in the UN’s global humanitarian pool, then trusted OCHA to allocate it. But in December, Jeremy Lewin, a senior official in the State Department, announced at a press conference that the administration would allow its contributions to the UN body to be spent only in an initial list of 17 countries, which included none of the seven whose current aid will soon end entirely. (According to Eri Kaneko, a spokesperson for OCHA, one more country has since been added to the list.) Lewin also announced that the U.S. would be contributing an initial $2 billion in 2026, far less than the country’s typical contributions.
The State Department spokesperson called OCHA’s pooled funding “a gold standard in flexible humanitarian funding.” But according to two senior humanitarian-aid experts and one State Department employee—who, like a number of people I interviewed for this story, asked to remain anonymous to discuss matters they were not authorized to speak about publicly, or because they feared the administration’s retribution—Lewin’s announcement blindsided State Department officials, embassy heads, and aid groups.
The nine other countries named in the internal State Department email appear to be included in the reworked partnership between the U.S. and OCHA. According to the email, the State Department will end lifesaving awards in those places, for reasons the email does not explain and the State Department spokesperson did not provide. (Ethiopia, Congo, and Kenya will be among the beneficiaries of Food for Peace, a program that was formerly part of USAID but is now, as of Christmas Eve, run by the Department of Agriculture.) The aid the selected countries receive through OCHA will come with new restrictions and monitoring requirements. According to guidance that OCHA distributed and I obtained, any American contributions to OCHA must be spent within six months of being donated. According to the two humanitarian experts, one based in South Sudan and the other in Washington, what groups will get this money and when any of it will be distributed is still hazy.
Since the December press conference, “the legal work of formulating formal awards for each recipient country has been taken forward rapidly,” Kaneko, the OCHA spokesperson, told me in a text message. “Extensive preparatory work has also been underway at both the country and global levels on the administration of this grant.” Kaneko defended the six-month deadline for spending, writing that, because several major countries have pulled back their contributions, “it is critical that these funds are translated swiftly into life-saving action for people who urgently need assistance and protection.”
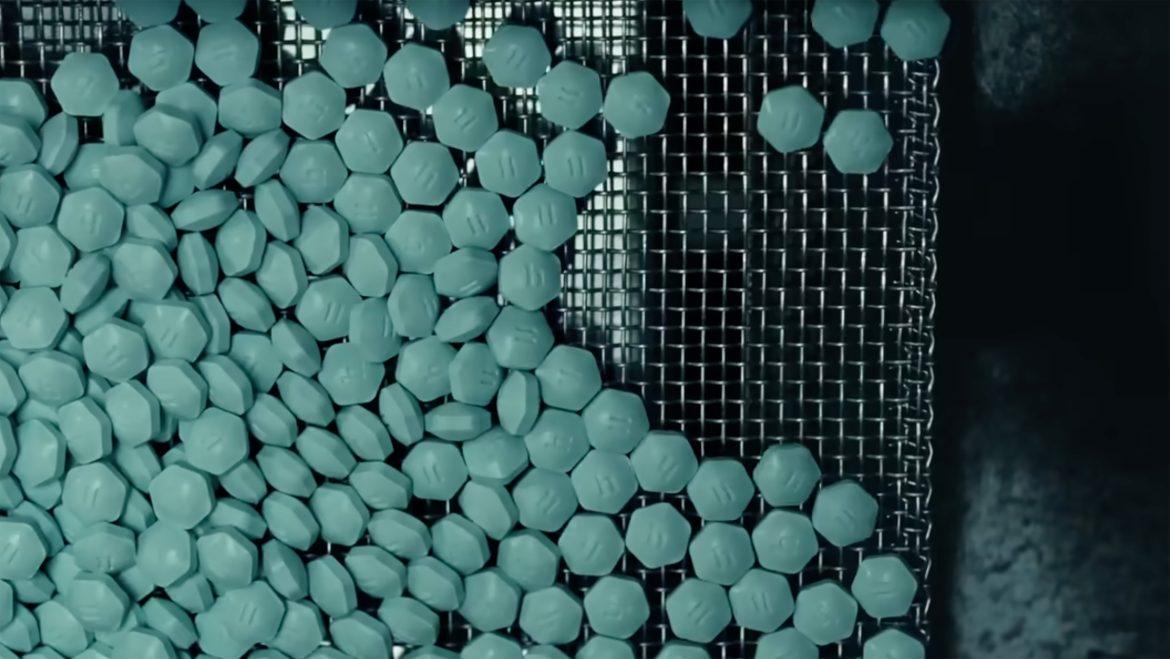
The aid programs being phased out this year were already notable for their continued existence. From January to March last year, the Department of Government Efficiency, led by Elon Musk, helped purge 83 percent of American foreign aid. Many more awards were canceled during a review by the White House’s Office of Management and Budget. The administration’s stated aims in so aggressively reducing foreign aid were to eliminate wasteful, “woke” awards while preserving work that it determined saved lives.
The administration’s definition of lifesaving was particularly strict. Funding for programs that fought tuberculosis and sent food to people who are chronically hungry, not yet starving, has been canceled. But stabilization centers that provide inpatient treatment to the most extremely malnourished children have generally, though not universally, been spared. Each of the newly canceled awards represents an occasion in which federal workers had previously convinced Trump appointees that the money would help meet the most basic survival needs of people fleeing war, caught in deadly disease outbreaks, or in danger of starving to death, a former senior State Department official, who left the administration in the fall, told me. “It has to be: ‘If we don’t deliver this, people die immediately,’” they said.
[Read: The world’s deadliest infectious disease is about to get worse]
Since the destruction of USAID last year, administration representatives have repeatedly insisted that lifesaving aid was being preserved. In March, Musk posted on X, “No one has died as result of a brief pause to do a sanity check on foreign aid funding. No one.” Secretary of State Marco Rubio has similarly claimed that reports of people dying because of USAID cuts were lies, and promised last spring that “no children are dying on my watch.” But reports of deaths that appear clearly linked to the cuts abound.
Conditions in some of the countries where aid is being canceled are already dire. Somalia, which will soon receive no American humanitarian funding at all, is undergoing a severe drought; earlier this year, analysts for the federal government reported that the hunger crisis is so extreme, it could deteriorate into full-blown famine by this summer. Hundreds of health and nutrition centers in Somalia shut down after last year’s steep aid cuts, according to Doctors Without Borders. In a regional hospital that Doctors Without Borders supports, deaths among severely malnourished children younger than 5 have increased by 44 percent, Hareth Mohammed, a communications manager working for the organization in Somalia, told me. Jocelyn Wyatt, the CEO of the Minnesota-based nonprofit Alight, which works in many countries affected by war or natural disaster, told me that her organization will have to close more than a dozen health facilities in Somalia in the next week, leaving as many as 200,000 people without any health care.
According to Wyatt, State Department officials had said in December that they were “optimistic” about funding for her organization’s work in Sudan being renewed in 2026. But last month, the State Department said the grant would actually end in February. Alight has run out of U.S. funding, and Wyatt told me that she has received no confirmation of if and when OCHA funds will materialize. (“We are working on allocating the funds as quickly as possible,” Kaneko said.) Alight has been forced to pull out of three refugee camps in Sudan, which Trump described on his social-media platform in November as “the most violent place on Earth and, likewise, the single biggest Humanitarian Crisis.” In nearly three years of civil war, more than 150,000 people have been killed in the country. The Trump administration maintains that genocide and famine are taking place there. Yet the global humanitarian effort to respond remains severely underfunded; this year, the World Food Program plans to reduce the rations it gives to people facing famine by 70 percent. Over the past month, Alight has closed 30 health clinics and 14 nutrition centers, and laid off more than 250 doctors, nurses, and staff members around Sudan, Wyatt said. In the three camps Alight exited, the organization had provided the only sources of health care. (The State Department spokesperson did not respond to questions about Alight’s funding.)
I spoke with an Alight worker who has been breaking the news of the sudden closures to people in displacement camps in Sudan over the past month, to sobs and disbelief. Many arrive at the camps wounded, and now the nearest health facility—a regional hospital—is a three-hour drive away from the camps through a war zone. “They are afraid,” the worker told me, of venturing into territory that’s rife with the same militants they have fled. Alight would drive refugees to the hospital when they presented with issues too severe to treat at the camps. But with the new cuts, the organization no longer has enough money to rent the cars.